Conversation Summary
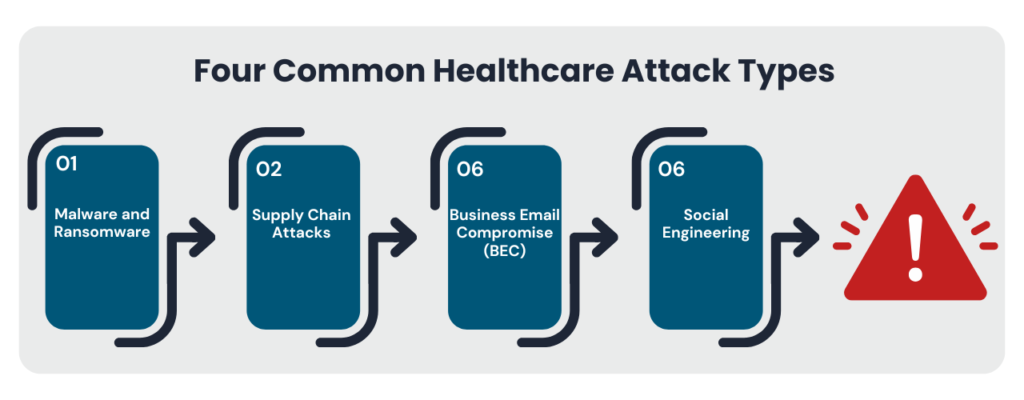
Amid the complexities of modern healthcare, where patient data and critical systems face relentless threats from sophisticated cyberattacks, penetration testing has become a cornerstone of an effective security strategy. As IT infrastructures grow increasingly more intricate—with Electronic Health Records (EHR) systems, telehealth platforms, IoT-enabled medical devices, and cloud-based solutions—all introducing potential vulnerabilities, penetration testing provides proactive protection against these risks. Unlike routine security measures, it simulates real-world cyberattacks to uncover hidden weaknesses such as unpatched software, misconfigured APIs, and insecure medical devices, addressing risks before malicious actors can exploit them.
This forward-looking approach not only bolsters compliance with stringent regulations like HIPAA and the HITECH Act but also ensures the integrity of interoperability standards such as FHIR-based APIs mandated under the 21st Century Cures Act. Through proactive identification of vulnerabilities, penetration testing delivers the critical insights needed to strengthen systems and protect against the most prevalent cyber-attacks.
Yet, despite its clear benefits, many healthcare providers still underestimate the importance of regular penetration testing, often unaware of the significant regulatory, financial, operational, and reputational costs a breach can entail. For healthcare organizations to fully appreciate the value of penetration testing, it’s essential to understand the hidden costs of neglecting it as a critical security measure and how routine testing can help organizations avoid these operational setbacks.
To start let’s examine why organizations in healthcare are particularly sensitive to cyber-attacks.
Why Healthcare Is Susceptible to Cyber Incidents
Healthcare has become an attractive industry for cybercriminals for several reasons. First, healthcare data is extraordinarily valuable on the black market. A patient’s health record can contain everything from Social Security numbers to insurance details and medical histories, making it worth up to 10 times more than other types of personal data.
Secondly, many healthcare systems rely on outdated technology, including legacy systems that are challenging to secure. A survey by HealthITSecurity found that nearly 80% of healthcare providers use outdated operating systems, which lack critical security updates and are more vulnerable to attacks. Moreover, as healthcare organizations integrate Internet of Things (IoT) devices to these outdated legacy systems, each new connection introduces a potential vulnerability. Cybercriminals are quick to exploit these vulnerabilities, often with devastating consequences for both patient safety and organizational operations.
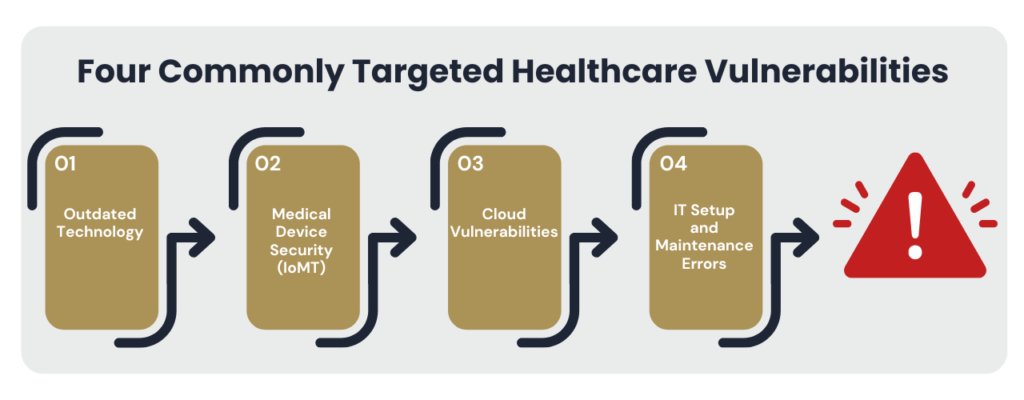
Penetration testing is a critical tool for identifying vulnerabilities in an organization’s network, systems, and devices before attackers can exploit them. By simulating real-world attacks, it reveals potential entry points for adversaries, enabling organizations to proactively strengthen their defenses, address outdated systems, and implement essential patches. Without robust and routine penetration testing, organizations risk exposing key components of their operations to cyber threats.
For healthcare organizations, the stakes are especially high. Data breaches in this sector can lead to severe operational disruptions, hefty financial penalties, and a loss of patient trust. According to IBM’s 2024 Cost of a Data Breach Report, the healthcare sector experienced the highest average breach cost of any industry, reaching an alarming $9.77 million per incident.
With these stakes in mind, it’s essential to explore the broader impact of neglecting penetration testing in healthcare, shedding light on its critical role in safeguarding operations and reputations.
Regulatory Fines and Compliance Penalties
For healthcare organizations, adherence to compliance standards is not only a legal requirement but also a safeguard for patient data. The Health Insurance Portability and Accountability Act (HIPAA) and the Health Information Technology for Economic and Clinical Health (HITECH) Act impose strict data protection requirements on healthcare providers. When a breach reveals non-compliance, regulators may issue substantial fines. For example, in 2020, the Office for Civil Rights (OCR) fined an insurance agency $6.85 million after a breach that compromised the data of 10.4 million individuals. The OCR determined that the organization had failed to conduct adequate risk assessments and implement sufficient security controls.
Penetration testing is a proactive step that can prevent breaches and resulting penalties by ensuring that healthcare systems meet regulatory standards. In fact, regular penetration testing is often viewed favorably by regulators, as it demonstrates a commitment to data security and compliance. Additionally, maintaining a record of proactive security measures, including penetration testing, can help reduce penalties if a breach does occur. For healthcare organizations, the cost of routine testing is a small price to pay to avoid the potentially devastating financial penalties associated with regulatory non-compliance.
Reputational Damage and Loss of Patient Trust
The impact of a cyber incident extends beyond immediate financial loss; it can also permanently damage patient trust. Healthcare providers are entrusted with highly sensitive information, and patients expect that their records will be kept safe. When a breach occurs, that trust is compromised. According to a survey by Accenture, nearly 25% of patients say they would consider changing healthcare providers if their data were compromised in a cyberattack. This translates directly to lost revenue, as patients choose competitors with better security practices.
The reputational fallout from a breach can affect not only patient retention but also partnerships with insurers, suppliers, and regulatory bodies. News of a security incident can have a long-lasting impact, making it challenging for the organization to regain its standing within the community. By conducting regular penetration tests, healthcare providers can identify and address vulnerabilities before they are exploited, thereby preserving both patient trust and organizational reputation.
Operational Downtime and Recovery Costs
Healthcare organizations are particularly vulnerable to operational disruptions during cyber incidents. Many healthcare providers rely on interconnected systems to deliver timely patient care. When these systems are compromised, the results can be catastrophic. One notable example is a 2017 ransomware attack that forced a major healthcare provider to cancel over 19,000 appointments, severely impacting patient care and resulting in millions of dollars in recovery costs.
The direct costs associated with operational downtime can include lost revenue, increased IT expenses, and overtime wages for staff involved in the recovery process. Indirectly, such disruptions can harm patient outcomes, as delayed access to medical records and treatment plans can worsen health conditions. In 2022, a study by the Ponemon Institute found that the costliest cyberattacks experienced by healthcare organizations resulted in an average financial impact of $4.4 million. This figure includes costs like lost productivity but does not factor in the actual ransom payments demanded by attackers. Routine penetration testing can significantly reduce these risks by identifying potential entry points for ransomware attacks, enabling healthcare providers to strengthen their defenses and maintain operational continuity.
Legal Costs and Potential Lawsuits
A healthcare data breach often invites legal action from patients, especially if compromised data is used in identity theft or fraud. The legal fallout from data breaches can be significant. For example, in 2021, a ransomware attack compromised the records of approximately 150,000 patients at a major healthcare provider, leading to a class-action lawsuit. The lawsuit claimed that the provider failed to implement sufficient security measures, underscoring the legal risks healthcare organizations face when data security is inadequate.
Legal fees and settlements add a significant financial burden following a data breach. Moreover, the absence of a proactive security strategy, including regular penetration testing, can make organizations appear negligent in court. Regular testing allows healthcare providers to demonstrate that they have taken reasonable measures to secure patient data, potentially reducing legal liabilities and settlement costs in the event of a breach.
Long-Term Remediation Expenses
The financial impact of a cyber incident often lingers long after the immediate recovery. For many healthcare organizations, addressing the underlying vulnerabilities exposed by a breach requires increased long-term spending on security measures. According to a Ponemon Institute report, nearly 60% of healthcare organizations increased their IT budgets following a data breach to address gaps in security infrastructure. This investment may include new cybersecurity tools, additional personnel, and comprehensive training programs.
By implementing regular penetration testing, healthcare organizations can address vulnerabilities before they are exploited, reducing the need for expensive post-breach remediation.
How Drummond Can Help You Avoid These Hidden Costs
Drummond’s healthcare-specific penetration testing services offer a comprehensive solution for identifying and addressing security vulnerabilities before they can be exploited. Our team of experts understands the unique challenges facing healthcare providers, from HIPAA compliance to the complexities of EHR systems. Drummond’s approach goes beyond standard testing; we focus on providing actionable, compliance-aligned insights that enable healthcare organizations to protect patient data and avoid costly incidents.
By choosing Drummond as your security partner, healthcare organizations gain access to tailored recommendations that can help reduce the risk of regulatory penalties, protect patient trust, and minimize the risk of operational disruptions. Our penetration testing services are designed to help you navigate the evolving threat landscape confidently, so you can focus on delivering safe and secure patient care.
Conclusion: Investing in Proactive Security
Ignoring penetration testing can lead to hidden costs that far exceed the expense of regular assessments. For healthcare organizations, the stakes are exceptionally high, as data breaches impact not only finances but also patient outcomes, operational integrity, and public trust. A single vulnerability can expose sensitive patient data, disrupt critical care services, and result in cascading consequences that affect an organization for years. The healthcare sector is unique in that it deals directly with human lives, and the inability to access patient information during a cyber incident can compromise the quality and timeliness of care.
For healthcare leaders who prioritize security, regular penetration testing represents a powerful step toward reducing the likelihood of costly breaches, regulatory penalties, and legal challenges. More importantly, it positions their organizations as trusted, reliable care providers who take every precaution to protect the privacy and well-being of their patients. Partnering with experts like Drummond can ensure that healthcare providers not only strengthen their cybersecurity posture but also foster a secure environment that upholds patient trust and supports long-term success in an increasingly digital healthcare landscape.
FREE CONSULTATION
And get answers for your most pressing penetration testing questions!
